Lymphedema
What Does Lymphedema Mean?
Lymphedema is due to abnormal lymph drainage by lymph nodes and lymph vessels. Lymph nodes filter fluid from bacteria, viruses and other foreign substances that are destroyed by special blood cells called lymphocytes. In lymphedema protein-rich fluid builds up, usually in an arm or leg. It causes swelling that can make it hard to use the swollen limb. (Figure 1) The limb is also more likely to be infected (erysipela). Lymphedema is a chronic and potentially debilitating condition but it can be very effectively managed and prevented! Unfortunately, due to a lack of awareness, information, and understanding, even within the medical community, lymphedema is often misdiagnosed or undiagnosed.
Figure 1 : Bilateral lymphedema of the lower limbs

There are 2 types of lymphedema :
- Primary lymphedema : Some people can get lymphedema for unknown reasons, probably congenital defects. Primary lymphedema can be present at birth (congenital), but most of the time it develops during puberty or in adulthood.
- Secondary lymphedema : Secondary lymphedema is often caused by cancer treatment. It is due to surgical removal of lymph nodes or to radiation, especially in breast cancer surgery. It can happen soon after surgery or radiation, but it more often occurs 1 or 2 years later, or even much later. Prevention of secondary lymphedema is a lifelong job.
Secondary lymphedema can also be caused by trauma with or without surgery. Sometimes it is caused by medicines.
Figure 2 : Lymphedema of the feet

Symptoms : Patients experience heaviness or fullness, swelling (edema) and sometimes aching in the affected limb. (Figure 2) In advanced lymphedema, there may be skin changes such as discoloration, verrucous (wart-like) hyperplasia (Figure 3), thickening of the skin (hyperkeratosis) and papillomatosis. In extreme cases, lymphedema can lead to elephantiasis. (Figure 4-5).
Figure 3 : Verrucous hyperplasia

Figure 4 : Elephantiasis

Figure 5 : Elephantiasis

Lymphedema should not be confused with other causes of edema (cardiac or renal failure, venous insufficiency etc). However, untreated venous insufficiency can be combined with lymphatic disorder leading to a mixed edema.
Staging : (according to the Fifth WHO Expert Committee on Filariosis) :
Stage 0 (latent) : The lymphatic disorder is not yet apparent.
Stage 1 (spontaneously reversible) : « non-pitting edema stage » (when pressed by the fingertips, the tissue bounces back without any indentation) : usually there is no edema upon waking.
Stage 2 (spontaneously irreversible) : « pitting edema » (when pressed by the fingertips, the affected area indents and holds the indentation). The edema has a spongy consistency. Fibrosis marks the beginning of the hardening of the limb.
Stage 3 : The swelling is irreversible and the limb can be very large. The tissue is hard and unresponsive.
Diagnosis : Imaging is not necessary to make the diagnosis of lymphedema, but it can be used to confirm it, to assess the extent of involvement, and to determine therapeutic intervention. Imaging may include the following:
1. CT-scan : to quantify lymphedema or when malignancy is suspected
2. Magnetic resonance imaging : idem
3. Ultrasonography : to evaluate the venous system and the subcutaneous thickening due to lymphedema
4. Lymphoscintigraphy : to evaluate the lymphatic system
Complications : It is vital for you to be aware of the symptoms of infection and to seek treatment at the first signs, since recurrent infections or cellulitis, in addition to their inherent danger, further damage the lymphatic system and set up a vicious circle. If you are not able to contact your GP (travel, week-end), start taking antibiotics before seeing him.
Figure 6 : Cellulitis
1. Infection : The protein-rich fluid accumulation interferes with healing and provides a rich culture medium for bacterial growth that can result in infection and in severe cases, to skin ulcers. Infection is usually due to skin lesions (trauma, cuts, mycotic infection…).
Bacterial infections :
- Erysipelas (cellulitis) : It is the most frequent infection in lymphedema. Patients have a rapid-enlarging red, swollen, warm, hardened and painful rash (orange peel-like) and develop general symptoms within 48 hours (high fever, fatigue, headache, vomiting). More severe infections can result in vesicles, bullae with possible skin necrosis and lymphedema worsening. Antibiotics should administered as soon as possible for a minimum 14 days, or until the inflammation has resolved. Usually hospitalisation is required. Non steroid antiinflammatory drugs and steroids should not be prescribed because of increased risk of necrotizing fasciitis. Erysipelas is different from non-infectious recurrent inflammation of the lympedematous limb that regresses spontaneously or under corticosteroid local application.
- The main portals of entry of erysipelas are intertrigo and wounds. Wound disinfection with an antiseptic (chlorhexidine or Betadine®) is recommended. Screening and treatment of a fungal infection, in particular, between the toes (intertrigo), is the most effective measure in terms of prevention of infectious complications. Treatment of such fungal infection is based on use of an imidazole cream or powder (Daktarin°).. If recurrence is frequent, long-term prophylaxis can be recommended. Use of an antifungal cream and appropriate skin care decrease the recurrence of erysipelas.
- Lymphangitis : It is the inflammation of the lymphatic vessels and channels caused by bacterial infections. A thin red line is observed running along the course of the lymphatic vessels acoompanied by the enlargement of the nearby lymph nodes. In the inferior limb it could be misdiagnosed as superficial venous thrombosis of the great saphenous vein.
- Necrotizing fasciitis (flesh-eating disease or flesh-eating bacteria syndrome) : It is a rare infection of the deeper layers of skin and subcutaneous tissues. Patients appear very ill. Without surgery and antibiotics, the infection will rapidly progress and eventually lead to death.
2. Cancer : Lymphedema can lead to cancer, but it is very rare.
Preveention and Treatment: Patients that have experienced lymph node removal and/or radiation for cancer should be careful and avoid lymphedema. Patients who already have lymphedema must take steps to avoid worsening and even to reduce it.
1. Prevention : Patients must be taught
a. How to recognize symptoms of limb swelling :
i. feeling as though clothes, socks, shoes or rings are getting too tight
ii. feeling as though the limb is getting heavier
iii. feeling less flexibility in the wrist, hand or ankle
b. How to avoid or reduce swelling :
i. Keep from wearing shirts with elastic cuffs (for upper limb lymphedema) or gartners or knee-high or thigh-high stockings (for lower limb lymphedema) except if you wear compression stockings
ii. Don’t use heating pads on the area, stay out of saunas and hot tubs because heat may make swelling worse.
c. How to exercise right the limb that is affected and how to avoid overuse of the limb
d. How to protect the limb from injury and infection because even a small infection can lead to serious lymphedema :
-
- Treat immediately any cuts, scratches, insect bites or other injuries
- Use sunscreen to protect your skin from sunburn
- Use insect repellent to protect the skin from insect bites
- Protect the affected arm from needle injections; don’t have blood drawn from that arm
- Do not allow a blood pressure cuff to be placed on the arm
- Wear gloves when gardening (for upper arm lymphedema)
- Use a thimble when you sew (for upper arm lymphedema)
- Take good care of skin and nails ; don’t cut cuticles
- Use a moisturizer because dry and cracked skin can get infected
- Use an electric razor for arm or leg shaving
- Keep feet clean : bathe feet in lukewarm, not hot, water ; use a mild soap
- Wear comfortable and supportive shoes that fit properly (for lower limb lymphedema)
- Wear clean socks or stockings everyday and don’t walk barefoot, especially outside even in the summertime (for lower limb lymphedema)
e. Check feet often for How to recognize infection : see the doctor at the first sign of a rash, pain, swelling or inflammation
i. Cuts, mycosis or infection
2. Treatment : Treatment varies depending on the severity of the edema and the degree of fibrosis. Although a combination treatment program may be ideal, any of the treatments can be done individually.
Figure 7 : Bandaging

a. Elevation of the affected limb can help
b. Skin care
c. Compression :
- Garments : elastic and/or non elastic garments.
- Compression bandaging (« wrapping ») : It utilizes several layers of padding and short-stretch (non elastic) bandages. (Figure 7) These bandages enhance the pumping action of the lymph vessel during exercise or daily activities. They help to soften fluid-swollen areas.
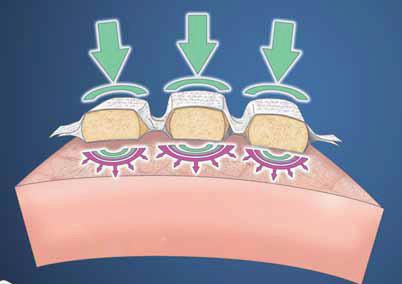
- Sequential gradient pump therapy : It utilizes a multi-chambered pneumatic sleeve with overlapping cells to promote movement of lymph fluid and help soften fibrotic tissue in the affected limb. It should only be used in addition to compression bandaging and manual lymph drainage. There have been reports linking pump therapy to an increased incidence of edema of the proximal part of the limb, such as genital edema. That is the reason why it should be preceded by manual proximal lymph drainage.
- Manual lymph drainage : It consists in gentle, rhythmic massaging of the skin to stimulate the flow of lymph. It can help to move fluid out of the swollen limb especially if the edema is not too fibrotic. The drainage lasts approximately 40 to 60 minutes. It must be associated with compression bandaging. Ask your doctor to refer you to a physical therapist who specializes in lymphedema.
- Chronic phase treatment : Once the lymphedema will be reduced, you will be asked to use elastic compression stockings and/or nonelastic directional flow foam garments and do gentle exercise in order to reduce swelling.
- Mobiderm°- Caresia° : They consist of foam cubes inserted between 2 layers of material. It is combined with elastic compression or non-elastic support and with variations in muscle volume (limb movements). It creates a shear effect on the indurated subcutaneous tissues. It is contraindicated in case of inflammation or infection of the limb or in cas of fragile skin. If the skin is fragile, a cotton bandage must be placed between Mobiderm° and the skin or this techniques must be avoided.

d. Become a member of a patients association : Due to a lack of knowledge, even within the medical community, patients are often left alone. This chronic disease can lead to severe psychological distress. Being a membre of a patients association can help you to understand and treat your lymphedema and get a much better quality of life.
e. Surgery : Prior to any surgery, patients should have been treated medically as described above. Lymphatic surgery is still debated and limited to specialised centers.
